![[BKEYWORD-0-3] A major failure of reconstruction was that](https://blackthen.com/wp-content/uploads/2015/07/failure-of-reconstruction.jpg)
A major failure of reconstruction was that - pity, that
OTES Preface 1. Thomas J. See also Jeanne F. Theoharis and Komozi Woodward, eds. Leslie A. Price, Jr. a major failure of reconstruction was thatA major failure of reconstruction was that Video
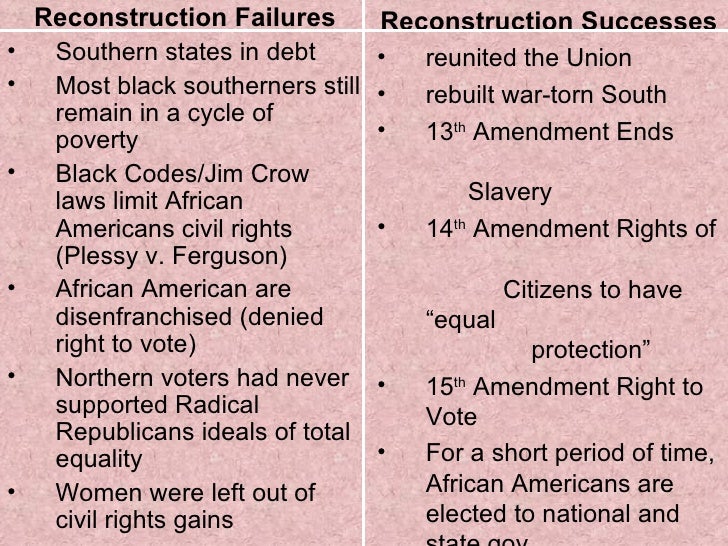
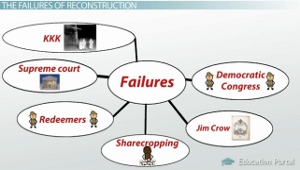
Failures of Reconstruction LectureA major failure of reconstruction was that - pity
The FDA Published the Following Directives to Patients and Caregivers Concerning Breast Reconstruction Patients who are electing breast reconstruction or augmentation surgery should discuss the risks, benefits, and possible complications connected with ADM products with their surgeon. Also, patients should discuss with their physician which type of ADM will be used during their surgery. ADMs are often used in other reconstructive surgeries such as hernia repairs. However, the FDA states that the off-label use of ADM products in breast augmentation or reconstruction procedures is not cleared or approved by its agency. The product is manufactured by removing cells while leaving the supportive tissue structure in place. While surgical products like FlexHD are cleared and approved by the FDA for some surgical procedures, such as hernia repair surgeries, there is little known about the possible complications of products such as FlexHD. The FDA affirms that FlexHD and ADM products vary significantly in their level of sterility, source material, final product state, biomechanical properties, processing, level of sterility, thickness, and preparation methods prior to surgical application. Some manufacturers even market their AMD products for use in breast reconstruction operations.The SMIF was raised as follows: The patient is positioned in extended supine position, and the required flap size is marked in elliptical shape 1 cm below the inferior border of the mandible. The flap is centered over the ipsilateral anterior belly of the digastric muscle with its perforators.
Skin laxity is checked by means of a pinch test to achieve primary closure without any tension incisions up to 6 cm in width are easy to close. The upper incision runs through the skin, the subcutaneous tissue, and the platysma 1 cm below the mandibular border measured from the mandibular angle to the chin.
Navigation menu
First, the facial vein comes into view at the middle portion of the submandibular gland, which is removed to access the submandibular groove. Here, the submandibular vessels and the cranially running marginal branch of the facial nerve come into view. The nerve is preserved, and the preparation runs on the mylohyoid muscle in anterior direction, clipping small branches, and dissecting the adjacent lymph nodes at level 1b. Reaching the osseous fixation of the anterior belly of the digastric muscle at the chin, the muscle fibers are cut off, and the harvested muscle belly is sutured to the flap skin to prevent shearing of the perforators. Now the flap is circumcised, and the tendon of the anterior a major failure of reconstruction was that muscle is cut off from the hyoid bone. Finally, the adjacent lymph nodes at level 1a are carefully dissected, preserving the perforators.
If more flexibility of the flap is needed, the vascular pedicle is dissected down to the origin of the facial artery at the upper border of the posterior belly of the digastric muscle and the facial vein down to the internal jugular vein.
The flap is temporarily reattached to the cranial skin flap, which allows completion of the neck dissection procedure. For intraoral reconstruction, the flap is passed behind the mylohyoid muscle into the oral cavity. Reconstruction of facial defects requires a wide subcutaneous tunnel to minimize pressure on the pedicle at the angle of the mandible. A subcutaneous passive drain prevents compression by hematoma. The donor site defect is closed by advancing the subplatysmal-undermined inferior skin flap, and excess skin is removed according to Burow. A clinical case with intra- as well as postoperative photo-documentation is shown in Figs.
Cite this page
For univariate analysis, chi-square tests were used to compare different groups of hhat parameters. The t-test two-sided was used for comparison of mean values. Results Table 1 comprises general patient data including specific information on associations between distinct flap types and clinicopathological factors. In the PMMF group, Additionally, alcohol abuse was significantly more prevalent in the Ws Patients in the PMMF group had more frequently a history of head and neck surgery Regarding the recipient flap site, the SMIF was used for different intra- and extra-oral sites whereas the RFF was predominantly used for tongue and floor of mouth reconstructions The PMMF was frequently chosen for mandible The PMMF With regard to the tumor T -stage classification a major failure of reconstruction was that malignancies, the PMMF was used for patients with more advanced stages In contrast, only Major perioperative complications occurred in 18 In 4 patients, arterial here led to severe perioperative complications, and 1 patient additionally developed serious wound infection.
Introduction
However, no significant association was found between complications and the type of flap. History of nicotine abuse Wound healing disorders were highest in the PMMF Overall flap success was Flap failure was associated with previous surgery Table 2 presents associations between the type of flap and treatment-specific factors. Mean flap size was larger in the PMMF Figure 2 shows associations between the used flaps and patient comorbidity. Patients in the SMIF mean score 5. Discussion Free flap reconstruction currently represents the first choice in managing complex maxillofacial defects because their functional and esthetic results and donor site morbidity rates are better than those of pedicled flaps [ 11 ].]
Also that we would do without your brilliant idea
Bravo, this excellent idea is necessary just by the way