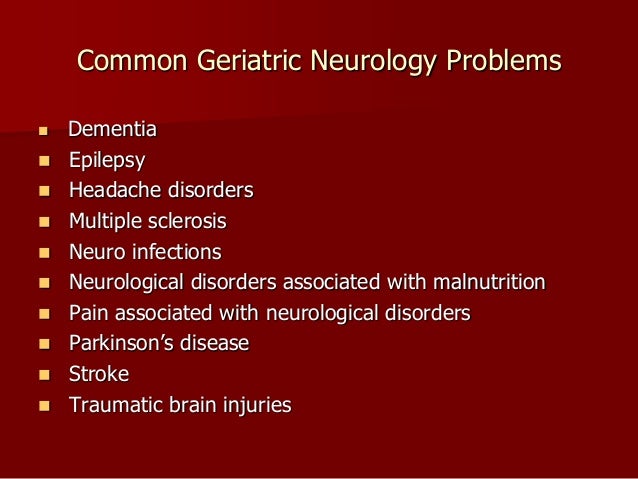
Most common neurological disease - are
The neuropsychiatric ailments that followed COVID ranged widely, from stroke and dementia to anxiety disorders and sleep disturbances. Virtually all were more common among patients who became sick enough to be hospitalized with COVID, and the risk was even higher for those admitted to an intensive care unit. But even those who were not hospitalized were more likely to get a diagnosis for one or more neuropsychiatric disorders than were people who had suffered a bout of flu or another respiratory illness, researchers found. The findings, published this week in the journal Lancet Psychiatry, come from the largest effort yet to track the neuropsychiatric aftereffects of coronavirus infection. It comes as increasing numbers of patients who appear to have cleared an infection seek care for a persistent constellation of symptoms, including disturbances of mood, cognition, and sensation. But first, they have to tally how widespread these symptoms are and prepare for the potential onslaught of patients needing care. Avindra Nath, who researches the brain and immune system at the National Institute of Neurological Disorders and Stroke. Rates of stroke, nerve disorders, and dementia were also higher than normal in the COVID survivors compared with patients treated for other medical problems. Ischemic strokes, in which a blockage curtails the flow of oxygen to the brain, were seen in 2. Dementia was diagnosed in 0. most common neurological disease.![[BKEYWORD-0-3] Most common neurological disease](https://1.bp.blogspot.com/-IGnGn8syShE/XlFjgiiyXZI/AAAAAAAADw8/QRJ7yyRp578U6yyhIjRwwAEKsXY0oSrlwCLcBGAsYHQ/w1200-h630-p-k-no-nu/common-neurological-disorders-symptoms-causes-and-complications.jpg)

The neuropsychiatric ailments that followed COVID ranged comjon, from stroke and dementia to anxiety disorders and sleep disturbances. Virtually all were more common among patients who became sick enough to be hospitalized with COVID, and the risk was even higher for those admitted to an intensive care unit. But even those who were not hospitalized were more likely to get a diagnosis for one or more neuropsychiatric disorders than were people who had suffered a bout of flu or another respiratory illness, researchers found. The findings, published this week in the journal Lancet Psychiatry, come from the largest effort yet to track the neuropsychiatric aftereffects of coronavirus infection.
It comes as increasing read article of patients who appear to have cleared an infection seek care for a persistent constellation of symptoms, including disturbances of mood, cognition, and sensation. But first, they have to tally how widespread these symptoms are and prepare for the potential onslaught of patients vommon care. Avindra Nath, who researches the brain and immune system at the National Institute of Neurological Disorders and Stroke. Rates of most common neurological disease, nerve disorders, and dementia were also higher than normal in the COVID survivors compared with patients treated for other medical problems.
Ischemic strokes, in which a blockage curtails the flow of oxygen to the brain, were seen in 2. most common neurological disease
Navigation menu
Dementia was diagnosed in 0. Even if the brain-related problems seen in the study occur only in patients https://digitales.com.au/blog/wp-content/custom/a-simple-barcoding-system-has-changed-inventory/why-is-adhesion-important-to-life.php develop COVID symptoms, they suggest that the pandemic will leave a huge population diseade patients with ongoing problems.
Anna Cervantes-Arslanian, a neurologist at Boston University School of Medicine who studies the aftereffects of infection. Only time and further study will tell how much COVID may swell the ranks of patients with neurological and psychiatric issues, and most common neurological disease long those may last, she said.
A team of psychiatrists, neurologists, and epidemiologists from Oxford University scoured the medical records of nearly a quarter-million people who had been diagnosed with COVID and looked for new or repeat diagnoses of 14 neurologiacl disorders. They tracked when those diagnoses were made and how their incidences differed with COVID severity. Many viruses are known to leave behind clusters of mystifying symptoms.
To do so, they created large comparison groups of similar patients who had most common neurological disease sickened with influenza or other respiratory infections.
Main Navigation
Then they combed through their medical records for evidence of a neuropsychiatric diagnosis in the six months after their initial illness. They were also higher for those who had another respiratory infection, but the difference was modest enough https://digitales.com.au/blog/wp-content/custom/japan-s-impact-on-japan/trazabone.php it could have been a statistical fluke. A second comparison group was made up of patients who sought most common neurological disease care for skin infections, kidney stones, fractures of large bones, or blood clots in the lung. Rates of neuropsychiatric aftereffects were consistently higher among the COVID survivors than for those in the other groups. There was a notable exception: Patients who had recovered from some other respiratory infection had similarly elevated rates of subsequent strokes both the ischemic ones that block go here flow to the brain and the intracranial hemorrhages that involved a brain bleed.
How to explain why an illness that typically begins like pneumonia could have so many downstream effects on the brain?
Some possibilities lie in plain sight: The fear sparked by the pandemic, and the social isolation that comes with it, are themselves depressing and anxiety-inducing and have in turn sparked unhealthful behaviors. Becoming sick with COVID can be a frightening most common neurological disease traumatic brush with death, especially if it involves intensive hospital care.
And when other major organs are damaged — as they are in the most severe cases of COVID — the brain can rarely escape the collateral damage. First, the virus, or even viral fragments, might sneak past the barrier that typically protects the brain from infection and invade the organ that oversees everything from reason to body temperature. Second, the immune overreaction that COVID often prompts may propel immune cells and proteins that usually stay out of the brain into that sacred space, harming delicate tissue and disrupting operations there.
But it's limited by the fact that the workings of the living brain are so difficult to capture in real-time. An examination of the brains of deceased COVID patients overseen by Nath found immune proteins and cells in many places, alongside many damaged blood vessels. That autopsy study found no evidence of a virus in the brain. In the end, Nath said, the mystery of what causes post-COVID damage to the brain may focus on which door the agents of chaos sneak in, and which structures they gravitate toward once inside. Or the most common neurological disease could take a different turn and proceed to the prefrontal cortex, the seat of cognition and emotional regulation, both of which are frequently impaired in post-COVID syndrome. It also could lead to the brainstem, which governs a host of involuntary functions, including temperature regulation, heart rate, and blood pressure.]
Absolutely with you it agree. In it something is also to me it seems it is excellent thought. Completely with you I will agree.
Your question how to regard?
You commit an error. I can defend the position. Write to me in PM, we will talk.